Ultrasound of the sinuses is called echosinusoscopy in another way. This is one of the simplest and safest methods of examining the paranasal sinuses.
The indications for examination are:
- inflammatory diseases - sinusitis, frontal sinusitis and others;
- allergic reactions accompanied by profuse mucous secretions;
- curvature of the nasal septum and injury;
- inflammation of the inner lining of the nose of a purulent nature;
- foreign body, tumor and neoplasm;
- damage to the mucous membrane.
In some medical centers, nasal ultrasound can be done around the clock. This allows children in urgent need of an urgent ultrasound scan of the sinus and check the fluid level in it.
This type of examination is needed to diagnose pathologies and diseases of the sinuses, including those accompanied by nasal congestion, mucous discharge, sinus swelling and other symptoms.
Survey technique
For the study of the nasal sinuses, an echosinuscope is used. This is an ultrasound scanner that allows you to assess the state of the environment and see neoplasms.
The examination is carried out using high-frequency sound waves, they are not perceived by the human ear. Passing through the sensor, they are converted into a graphic image.
AND Instructions for performing an ultrasound examination of the sinus may look like this:
| The patient should take a sitting position. This will allow the doctor to get initial information about the condition of the sinuses and determine the level of fluid in them. |  |
| The doctor lubricates the area to be examined with a gel and presses the sensor against the skin. During the examination, the patient should tilt his head in different directions, because if there is pus or fluid, then it will move. |  |
| The echosinuscope displays information about the condition of the sinus. After receiving the image, the doctor releases the patient and evaluates the result. |  |

Diagnostics takes no more than 15 minutes.
Note. When examining a child's sinuses, a different sensor is used than for adults, and a gel with a different composition, which enhances visualization to a greater extent.
Information is displayed in the form of a graphic image. During the examination, the ultrasound beams deviate from their path. They can be absorbed or reflected, depending on the environment they enter. All changes are visible on the curve that the doctor is studying.
How the information is displayed on the echosinuscope can be seen in the video for this article:
Survey results
What does ultrasound of the paranasal sinuses show?
You can see all the pathological changes, namely:
- neoplasms in the form of cysts and polyps;
- Pus or fluid in your sinuses
- foreign bodies;
- soft tissue diseases such as boils, carbuncles, and lipomas.
Ultrasound helps determine the size, as well as control the dynamics of growth of neoplasms. It allows you to monitor the treatment process, observe changes for the better or worse, and promptly adjust the therapy.

This is one of the reliable ways to prevent the development of complications, for example, when the fluid does not leave the sinus, but accumulates there for a long time, then the inflammatory process can rise higher, on the head.
Also, the survey allows you to determine the following parameters:
- condition of the mucous membrane and subcutaneous tissue;
- cartilage parameters;
- the thickness of the walls of blood vessels;
- the intensity of blood circulation.
Fluid in the sinuses
Fluid can accumulate in any of the paranasal sinuses, depending on which one is affected by the inflammatory process. Conventional ultrasound diagnostics can detect the presence of excess fluid in the sinuses.
With the help of an echosinuscope, you can determine the following parameters:
- volume of content;
- localization and boundaries of fluid;
- one - or two-sided defeat.
To identify fluid in the sinuses, the patient must alternately take two positions: first lying on his back, and then on his stomach. This will allow for the primary differential diagnosis between the accumulation of discharge and masses.
Note. An ultrasound scan should be done regularly to monitor the level of the sinus contents.
Also, the doctor may prescribe Doppler sonography to the patient. This subtype of ultrasound diagnostics allows assessing the blood supply to the sinus.
Ultrasound of the paranasal sinuses is not as popular as X-ray or CT, but it is indispensable for diagnosing children and pregnant women. It can be used as a primary diagnostic method for prescribing treatment.
Air cavities in the body of the upper jaw, as well as in the frontal, ethmoid and sphenoid bones are called paranasal sinuses. In the early stages of intrauterine development, outgrowths appear from the mucous membrane of the nasal passages, which, as they grow, invade the corresponding bones, forming air sinuses. Each sinus communicates with the nasal cavity. The maxillary sinuses are usually well developed at birth, the frontal and sphenoid sinuses develop by 6-7 years of age, and the ethmoid labyrinth at puberty. Thus, the sinuses are fully formed by the age of 17-20.
The maxillary (maxillary) sinus is located in the body of the upper jaw. Although the maxillary sinuses appear rectangular in lateral view, they have the shape of a truncated trihedral pyramid with an apex close to the zygomatic process. The maxillary sinus has five walls: upper, lower, internal, posterior, and anterior. The two maxillary sinuses vary considerably in size and shape, but are usually symmetrical. The sinus may be separated by incomplete or complete septa. The maxillary sinuses communicate with the middle nasal passage.
The frontal (frontal) sinuses are located in the frontal bone of the skull to the left and right of the midline. The frontal sinus is bounded by four walls: anterior, posterior, inferior, and internal. The septum between the sinuses usually deviates from the midline, so the frontal sinuses are rarely symmetrical. Sometimes they are missing. Inside the frontal sinuses, there may be bony protrusions and septa. Like the maxillary sinuses, the frontal sinuses communicate with the middle nasal passage.
Click on the picture to enlarge.
 |
On ultrasound, the superficial frontal and maxillary sinuses are clearly visible, the ethmoid labyrinth cells are partially visible through the eyeball, and the sphenoid sinus is inaccessible. Ultrasound allows you to determine the presence of air, fluid or thickened mucous membrane in the sinus, as well as track the dynamics of the pathological process during treatment. ENT doctors use ultrasound for primary screening and dynamic observation of the pathology of the frontal and maxillary sinuses.
Sinuses on ultrasound
For ultrasound of the sinuses, a high-frequency linear transducer of 7.5-13 MHz is used. But research can be done with any type of sensor.
| Photo. An image of the maxillary sinuses obtained using different types of transducers: A - convex transducer, B - linear transducer, C - cardiac transducer, D - pediatric transducer. |
 |
The examination of the paranasal sinuses is best done with the patient in a sitting position with a slight tilt of the head forward. Additional positions with tilting the head back, as well as tilting forward and to the side will help distinguish effusion from other pathological conditions.
The examination of the maxillary and frontal sinuses is always carried out in the transverse and longitudinal planes. It is especially important to compare the results on the right and left side. To examine the maxillary sinus, the transducer is placed under the inferior wall of the orbit and then scanned parallel to the inferior edge of the orbit from top to bottom. Note that the distance to the posterior wall of the maxillary sinus decreases as you move from the orbit to the alveolar process. The transducer is then rotated and scanned mediolaterally. To study the frontal sinus, the sensor is placed on the bridge of the nose.
Due to the change in impedance between soft tissues and bone, as well as between bone and air, ultrasonic waves are completely reflected behind the anterior wall of the air sinus. Thus, when scanning a healthy sinus, the first layer is represented by skin and subcutaneous tissue, then a thin continuous hyperechoic anterior sinus wall is determined, followed by thin parallel echo lines from multiple reflections of ultrasound waves back to the transducer. Reverb artifact should not be confused with back wall reflection.
| Photo. Transverse section of the mandibular air sinus on ultrasound: A - only the front wall is visible with minimal reverberation artifact; B, C - the reverberation artifact behind the front wall is more pronounced; D - a mirror image with a single A-line can be mistaken for a thickening of the mucous membrane or the posterior wall of the sinus, but the A-line is not located deep enough from the anterior wall (in our case, only 1.4 cm). |
 |
The walls of the sinus are visible only in the case of pathological conditions. When the sinus is filled with fluid or thickened mucosa, or when polyps are in direct contact with the anterior wall, ultrasound waves continue in depth and can be reflected at the posterior and lateral walls. The posterior wall in the maxillary sinus in adults is usually located at a depth of about 40 mm, and in the frontal sinus - 20 mm.
Pathology of the maxillary and frontal sinus on ultrasound
Sinusitis is an inflammation of the sinus mucosa due to infection or exposure to allergens and other pathogenic factors. In acute inflammation, the mucous membrane swells and effusion appears. In a chronic process, the mucous membrane is sharply thickened, effusion, cysts or polyps may be present.
How to interpret ultrasound data of maxillary sinuses:
- Normal sinus: soft tissues (skin and subcutaneous tissue); hyperechoic anterior wall with reverberation artifact (A-lines) behind; the back and side walls are not defined.
- "Incomplete sinusogram": soft tissues (skin and subcutaneous tissue); hyperechoic anterior wall; a bright hyperechoic V- or U-shaped contour of the posterior wall is clearly visible; side walls are not defined; the cavity looks hypo- or anechoic. An "incomplete sinusogram" is recorded on ultrasound if the sinus is partially filled with effusion or the mucosa is concentrically thickened. When the mucosa is noticeably thickened, the posterior wall is defined at a distance< 3,5 см у взрослых и < 2 см у детей.
Important!!! An effusion that does not completely fill the sinus may become visible when the head is tilted forward and disappear after straightening. It takes some time to drain the jelly-like exudate.
- "Complete sinusogram": soft tissues (skin and subcutaneous tissue); hyperechoic anterior wall; U- or V-shaped contour of the back wall and side walls form a clear triangle; the cavity looks hypo- or anechoic. On ultrasound, a "complete sinusogram" is recorded if the sinus is filled to the brim with effusion. A retention cyst differs from a sinus with effusion in that the posterior wall appears to be rounded and spaced apart< 3,5 см у взрослых и <2 см у детей
Important!!! When assessing the maxillary sinuses, the results of ultrasound and radiography coincide in 80% of cases. But sometimes, with a normal ultrasound picture, a moderate concentric thickening of the mucous membrane is determined on the roentgenogram, and with normal roentgenograms, incomplete sinusograms on ultrasound.
| Photo. A "complete sinusogram" on ultrasound may correspond to a sinus filled to the brim (A) or a retention cyst (B). Note that in the case of effusion, the V-shaped posterior wall is at a depth of 3.5 cm from the anterior wall, and in the case of a retention cyst, the rounded posterior wall is at a depth of 1.5 cm from the anterior wall. | ||
 |
 |
|
| Photo. On ultrasound, a transverse section of the maxillary sinus: A - Healthy air sinus. B, C - The posterior wall of the sinus is only partially visible, which can be interpreted as a small amount of fluid or thickening of the mucous membrane. D - An "incomplete sinusogram" with a bright V-shaped back wall indicates fluid level. |
 |
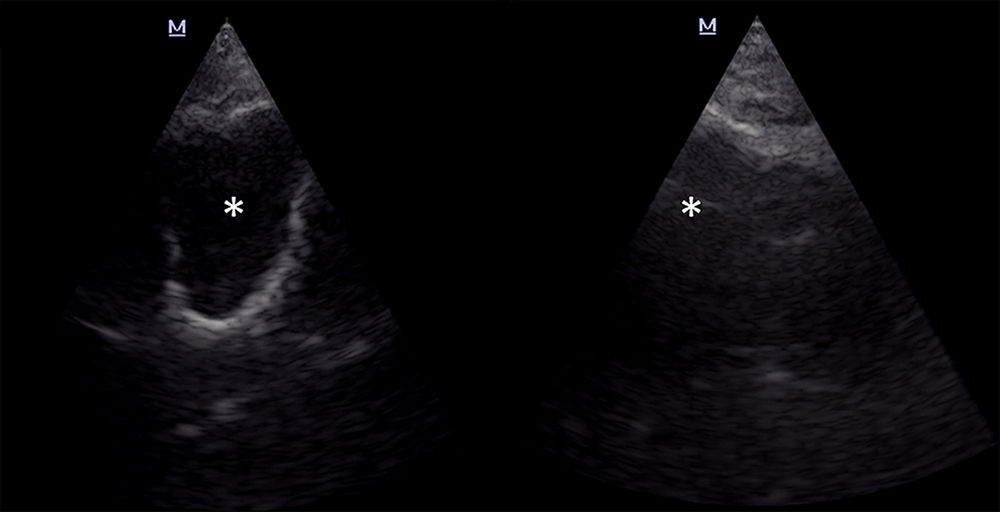
| Photo. A man with aspiration pneumonia and acute respiratory distress syndrome who is fed through a tube inserted in his left nostril developed fever and purulent nasal discharge. On ultrasound of the maxillary sinuses: all the walls of the sinus are clearly visible on the right, the cavity (asterisk) is almost anechoic; the walls on the left are not determined, the cavity (asterisk) is echogenic. Conclusion: A "complete sinusogram" indicates that the right maxillary sinus is completely filled with exudate. During the puncture, purulent-hemorrhagic contents were obtained. Culture is positive for Candida albicans and Pseudomonas aeruginosa. |
 |
| Photo. A 37-year-old man with complaints of headaches in the forehead. The left maxillary sinus on ultrasound: the back and side walls are clearly visible on the transverse section (A), along the side walls an echogenic strip is determined (probably mucous), the cavity is hypoechoic; on a longitudinal section, an echogenic strip (probably mucous) is clearly visible along the anterior and posterior walls. Conclusion: Echo signs of hypertrophy of the mucous membrane of the left maxillary sinus. On CT (B), the mucous membrane of the left mandibular sinus is noticeably thickened. |
 |
| Photo. During the initial examination on ultrasound, a "complete sinusogram" of both maxillary sinuses is determined, which indicates bilateral sinusitis. Against the background of therapy on ultrasound, positive dynamics. However, even after 2 months, the contour of the posterior wall is determined in the right maxillary sinus, which can be interpreted as a thickened mucosa. |
 |
| Photo. Maxillary sinuses on ultrasound and MRI: An “incomplete sinusogram” on the right corresponds to a retention cyst on an MRI, and a normal ultrasound picture on the left corresponds to a small fluid level on an MRI. |
 |
Video. The sensor is located transversely between the eyebrows. Ultrasound reveals a thick hyperechoic anterior wall and a flat-curved posterior wall at a depth of 1.5 cm. Conclusion: Echo signs of frontal sinusitis. Important!!! A mirror image with a single A-line can be mistaken for an echo of the back wall.
Take care of yourself, Your Diagnostician!
The pathology of the paranasal sinuses (SNP) in recent years has come out on top in the structure of diseases of the ENT organs, and the share of maxillary sinusitis among other sinusitis is 56-73%. An otolaryngologist at an outpatient appointment most often deals with different types of acute and chronic sinusitis, therefore, the diagnosis of these conditions is extremely important.
The most common symptoms of sinusitis are facial pain, difficulty in nasal breathing, purulent nasal discharge, and impaired sense of smell. More often pains are localized in the frontal region, less often - in the zone of projection of the maxillary sinus, sphenoiditis is characterized by pain in the back of the head and in the depths of the head, the appearance of an unpleasant odor in the nose, the flashing of flies before the eyes, convergence disorder, decreased vision, dizziness, nausea and even vomiting. These symptoms are due to the location of the sphenoid sinus at the base of the skull and the close proximity of the brain, optic, blocky, oculomotor and abducens nerves. It is known that monosinusitis - a lesion of one sinus - is a rare pathology. With sinusitis, as a rule, there is a lesion of several sinuses at the same time, and the symptoms of the pathological process in any sinus may prevail, masking the defeat of other paranasal sinuses.
Certain problems arise in the differential diagnosis of sinusitis with allergic rhinitis, which is often accompanied by significant swelling of the mucous membrane of the paranasal sinuses.
Anterior rhinoscopy, plain radiography and diagnostic puncture of the maxillary sinus, as well as bacteriological and cytological examination of secretions from the nasal cavity are traditional in the diagnosis of sinusitis, in some cases diaphanoscopy is used.
Anterior rhinoscopy makes it possible to judge the presence of sinusitis when a mucopurulent secretion is detected in the region of the middle nasal passage, but its absence does not exclude a pathological process in the sinuses.
Diaphanoscopy (transillumination), when compared with plain radiography, often gives false negative results, its use is limited to the maxillary and frontal sinuses and cases of edema of the sinus mucosa.
Optical endoscopy of the nasal cavity has become widespread in recent years. The method clarifies the data of standard diagnostic techniques, helps to investigate the patency of the sinus anastomoses, but does not provide direct information about their contents.
Infrared thermography, microwave radiometry, histography for various reasons have not found wide application in practice; rhinomanometry is intended to study the function of nasal breathing and supplements the information obtained by imaging methods.
Diagnostic puncture of the maxillary sinus is widely used and allows you to get the contents of the maxillary sinus or prove its absence, but this method does not give an idea about the condition of the walls and mucous membrane of the sinus, about the presence of polyps and other formations in it. In addition, the negative quality of this method is its invasiveness.
Plain X-ray is the most common method for diagnosing SNP pathology, despite the fact that the ethmoid labyrinth cells and the sphenoid sinus are of limited access to it. Often, the method gives false positive results when examining the maxillary and frontal sinuses. The inconsistency of the results of plain radiography and computed tomography ranges from 23 to 74%.
Computed tomography is the gold standard in the diagnosis of sinusitis, providing information about the spatial relationship of the intranasal structures and all paranasal sinuses; computed tomograms serve as a map when planning a surgical intervention. However, this method is quite expensive, so its use is impractical in everyday practice to identify common forms of sinusitis and monitor conservative treatment.
At the same time, there are many examples when none of the methods of radiological diagnostics can be applied, and it is necessary to assess the state of SNP. This primarily applies to cases of acute or chronic sinusitis in pregnant women, in patients who have just had other x-ray examinations. In addition, sometimes patients fundamentally refuse X-ray examination. In such a situation, the method of choice is ultrasound examination of SNP.
Ultrasound scanning in A-mode using a sinuscope has been used for a long time in otolaryngology and in experienced hands has an accuracy of 76 to 90%, although it often does not allow differentiating a volumetric formation inside the sinus (cyst, polyp, mucocele) from edema of the mucous membrane and fluid component ... Diagnostic errors in this pathology are possible in 9 out of 10 cases due to the difficulties in interpreting the data obtained, in addition, the A-method does not allow to establish the nature of the secret and its consistency.
Ultrasound examination of the paranasal sinuses in B-mode (US) provides two-dimensional polypositional visualization of not only the paranasal sinuses, but also other bone structures and soft tissues, due to which a better topographic orientation and interpretation is achieved than with the A-method. The results of ultrasound in 100% of observations coincide with the data of plain radiography. So, according to V.V. Shilenkova et al. , Ultrasound is an alternative to plain radiography in the initial diagnosis of sinusitis of the maxillary sinus.
The aim of this work was to assess the clinical significance of ultrasound of the paranasal sinuses in the B-mode in the primary diagnosis and monitoring of conservative treatment of sinusitis in conditions of the impossibility of using plain radiography and computed tomography, in particular, during pregnancy.
Material and methods
The study included 26 patients (25 women and 1 man) aged from 26 to 60 years (mean age 34.6 ± 3.2 years), who consulted an otolaryngologist of the polyclinic, who underwent an ultrasound examination of the paranasal sinuses in connection with the fact that 23 patients were pregnant (period from 16 to 33 weeks), 2 patients on the day of treatment or the day before, an X-ray examination of the lungs was carried out, 1 patient refused an X-ray examination. All patients at the time of treatment were worried about nasal congestion (26 people), 17 - mucous discharge, 11 - mucopurulent discharge from the nose and nasopharynx. 23 patients complained of headache, 15 had subfebrile temperature (37.2-37.4 ° C). On examination, in all cases, various degrees of swelling of the turbinates, mucous or mucopurulent discharge in the nasal passages were noted, in 11 cases - curvature of the nasal septum, in 5 - adenoid vegetations in the dome of the nasopharynx. One woman had previously been operated on for polyposis sinusitis, two had suffered from chronic catarrhal sinusitis in the last 3 years. Clinical data required the exclusion of acute or exacerbation of chronic sinusitis.
Ultrasound was performed on modern ultrasound scanners with linear transducers with a frequency of 7.5 MHz with a working surface length of 37-40 mm in two mutually perpendicular projections: sagittal and horizontal, in a sitting position facing the doctor.
The study was carried out according to the method of V.V. Shilenkova et al. and began with a sagittal view of the maxillary sinus. Finding the lower wall of the orbit, which is the upper wall of the sinus, serves as a guide when searching for the sinus itself. The transducer was moved medially and laterally to inspect the corresponding lateral sinus walls. At the second stage, to obtain horizontal sections, the sensor was moved parallel to the lower edge of the orbit from top to bottom, taking into account that the distance to the posterior wall of the maxillary sinus decreases when moving from the bottom of the orbit to the alveolar process.
To examine the frontal sinus, scanning was started in the horizontal plane from the nose bridge, then sagittal sections were obtained.
The normal ultrasound picture of SNP is characterized by the absence of visualization of their posterior walls as a result of natural pneumatization (Fig. 1).
Rice. 1. Echographic picture of the maxillary sinus is normal, sagittal section: a - skin, b - soft tissues, c - air, thin arrows - anterior wall of the sinus.
The frontal sinus is located in the thickness of the frontal bone, in 10-15% of patients it may be absent, it has 4 walls: the lower orbital - the thinnest, the anterior - the thickest (up to 5-8 mm), the posterior, separating the sinus from the anterior cranial fossa and internal - partition. The volume of the sinus ranges from 3 to 5 cm³. The maxillary sinus is located in the body of the maxillary bone and is an irregular pyramid with a volume of 15 to 20 cm³.
The bony base of the anterior or facial wall of the maxillary sinus has a depression called a canine or canine fossa, and is visualized as a concave hyperechoic line, beyond which no structures are normally detected.
The soft tissues of the canine fossa are represented by skin, subcutaneous fat and facial muscles (Fig. 2). The most superficial is m. levator labii superioris alae nasi, going from the lower medial edge of the orbit to the upper lip, only its abdomen is visible on the echogram, since the place of discharge remains outside the cut. The middle position is occupied by m. levator labii superioris, starting from the entire infraorbital edge of the upper jaw, muscle bundles converge downward and enter the thickness of the muscle that raises the corner of the mouth and wing of the nose. The deepest is m. levator anguli oris, starting from the bottom of the canine fossa and attaching to the corner of the mouth.

Rice. 2.
Below the place of departure m. levator labii superioris hyperechoic line, which is a reflection of the bone surface, has a small "defect" corresponding to the infraorbital foramen (foramen infraorbitalis), through which the nerve and artery of the same name emerge from the infraorbital canal.
The upper wall of the maxillary sinus simultaneously represents the lower wall of the orbit, its position is quite well defined due to visualization of the orbit (Fig. 3).

Rice. 3.
The posterior wall of the maxillary sinus is bordered by the cells of the ethmoid labyrinth and the sphenoid sinus, its most distant point is located at a distance of 27 to 34 mm from the anterior wall, the medial wall is the lateral wall of the nasal cavity, the lower one is formed by the alveolar process of the upper jaw and is characterized by a close location of the roots of the teeth to the sinus cavity. In some cases, the tops of the roots of the teeth will stand in the lumen of the sinus and are only covered with a mucous membrane, which can contribute to the development of odontogenic infection of the sinus and the ingress of filling material into its cavity.
Visualization of the posterior wall is possible only in case of violation of the pneumatization of the sinus and depends on the amount of secretion or other contents: the less air in the sinus, the more complete the view of its walls will be. It should be borne in mind that sometimes there are bony ridges and bridges on the walls of the sinus, dividing the sinus into bays and very rarely into separate cavities.
results
In 8 patients, according to the results of ultrasound, SNP pathology was not revealed. In 18 cases, acute maxillary sinusitis was established: in 14 patients - with thickening of the mucous membrane of the sinus, including 2 with the presence of cysts, 2 more with the presence of polyps; in 6 patients - with the presence of exudate (in 1 woman with hyperechoic inclusions, with additional examination, it turned out to be filling material). Frontal sinusitis with thickening of the mucous membrane of the frontal sinus was diagnosed in 3 patients.
Taking into account the ultrasound picture, the appropriate treatment was selected and carried out. In the course of therapy, ultrasound of the SNP was repeated in all the examined patients, which made it possible to assess its effectiveness and make the necessary adjustments. All cases of acute sinusitis ended in recovery, with chronic processes it was possible to achieve remission. Subsequently, 5 patients after childbirth underwent computed tomography of SNP, which confirmed the presence of cysts in 2 cases, polyps in 2 and filling material in the maxillary sinuses in 1 patient.
With edema of the mucous membrane of the maxillary sinus behind its anterior wall, a zone of reduced echogenicity of a homogeneous structure with a fairly clear distal contour with a thickness of 0.5 to 1.6 cm appears (see Fig. 2).
The horizontal line of separation of the media, which would correspond to the X-ray concept of "liquid level", is not visible during ultrasound, since the ultrasound beam passes parallel to this border, no matter how we move the sensor. Consequently, the amount of exudate in the cavity has to be judged by the extent of visualization of the posterior wall, which corresponds to the level of fluid in the sinus (see Fig. 3, 4). An important detail of ultrasound is the correct position of the patient's head, it should not be tilted back, since in this case the secret in the sinus moves to the back wall, an air gap appears between the front wall and the secret, creating conditions for obtaining a false negative result.

Rice. 4.
In the study in dynamics against the background of treatment, as the amount of exudate in the sinus decreases, the length of visualization of the posterior wall decreases until its complete disappearance, which corresponds to the restoration of pneumatization.
If there is a cyst in the maxillary sinus (Fig. 5), one of the ultrasound symptoms may be a change in the contour of the anterior sinus wall, which becomes convex due to its alignment with the anterior wall of the cyst. The posterior wall of the cyst is visible as a hyperechoic line with a curvature, in contrast to the distal contour of the thickened mucous membrane, repeating the relief of the anterior sinus wall.

Rice. 5. Echographic picture of the maxillary sinus cyst, horizontal section: a - skin, b - soft tissues, c - air, thin arrows - the anterior wall of the cyst, thick arrows - the posterior wall of the cyst.
Inhomogeneous sinus contents, when grouped or scattered hyperechoic inclusions are visualized against the background of a thickened mucous membrane or exudate, which do not disappear with repeated examinations, is an indication for subsequent computed tomography to exclude polyposis or the presence of foreign bodies (filling material), which are often the development of sinus etiological factor ...
conclusions
In the primary diagnosis and in the monitoring of conservative treatment of sinusitis in a polyclinic, if it is impossible to use plain radiography and computed tomography for one reason or another, in particular in pregnant women, ultrasound examination of the paranasal sinuses in the B-mode is the safest, non-invasive diagnostic method, which gives an important information for clinicians and should be used on an outpatient basis in all cases.
Literature
- Gurov A.V., Zakarieva A.N. Possibilities of modern macrolides in the treatment of acute purulent sinusitis // Consilium medicum. 2010. 12.N 3. P. 31.
- Dobson M.J., Fields J., Woodford T.A. A comparison of ultrasound and plain radiography in the diagnosis of maxillary sinusitis // Clin. Radiol. 1996. No. 51. P. 170-172.
- Puhakka T., Heikkinen T., Makela M.J. et al. Validity of ultrasonography in diagnosis of acute maxillary sinusitis // Arch. Otolaryngol. Head Neck Surg. 2000. V. 126. P. 1482-1486.
- Revonta M. Ultrasound in the diagnosis of acute maxillary sinusitis // Abstracts of ERS and ISIAN. Tampere. Finland. June 11-15, 2006. P. 139-140.
- Shilenkova V.V., Kozlov V.S., Byrikhina V.V. Two-dimensional ultrasound diagnostics of the paranasal sinuses // Textbook. Yaroslavl, 2006.
Pathologies of the paranasal sinuses in ENT practice occupy one of the leading places in terms of detection frequency. The most common type of sinus disease is sinusitis, an inflammatory process. Approximately 35-45% of visits to otolaryngologists are associated with diseases of these bone cavities, which are also called the paranasal sinuses. Given the complex structure of the structure of the paranasal sinuses (four groups of sinus cavities are distinguished in humans), visual examination of the patient as a diagnostic method has low efficiency. Doctors use more specific methods of examining the paranasal sinuses, including ultrasound of the paranasal sinuses.
Ultrasound of the paranasal sinuses: how it works and why it is prescribed
The entire technique of the examination method is based on the properties of ultrasound beams. The biophysics of ultrasonic waves makes it possible to visualize and study the phenomena and processes found in the process of ultrasound passage through biological tissues. The doctor, carrying out the diagnostic procedure, examines the interaction of ultrasonic waves with biological tissues, and the mutual influence of tissues on ultrasound. This phenomenon is due to the piezoelectric effect. The category denotes a process in which ultrasonic waves, acting on the surface of single crystals of certain substances, create certain deformations and mechanical vibrations in them, emitting ultrasonic waves, at the same time, electric charges with the opposite sign appear on the surface of the crystals.
Ultrasound examination of the paranasal sinuses (another name is echosinusoscopy) allows you to use the properties of ultrasonic waves in order to study the condition of the sinuses, determine the presence or absence of pathologies and diseases, identify indications for the appointment of a surgical intervention, develop a treatment regimen, and monitor the effectiveness of medical or surgical treatment, and performed physiotherapy.
Human paranasal sinuses anatomy
 The paranasal sinuses are hollow air formations in the bones of the skull that are connected to various nasal passages.
The paranasal sinuses are hollow air formations in the bones of the skull that are connected to various nasal passages.
The formation of these bone cavities occurs during the intrauterine development of the fetus, and ends after the end of puberty. The inner surface of the hollow formations is covered with ciliated epithelium with goblet cells. Their main purpose is to produce mucus. The mucus moves to the openings of the sinuses due to the movement of the cilia of the epithelium.
There are four groups of paranasal sinuses in the human head:
- paired maxillary, or maxillary;
- paired frontal sinus;
- paired lattice labyrinth;
- unpaired sphenoid sinus.
The maxillary sinus, as the name implies, is located in the body of the upper jaw. The volume of the cavity in an adult can reach 30 cubic centimeters.
The cavity has an irregular shape, formed by four walls:
- front;
- top;
- bottom;
- internal.
Frontal sinuses are cavities in the thickness of the frontal bone of the skull, located corresponding to the brow ridges. The shape of these sinuses is a triangular pyramid with a base directed downward. The volume of the cavity in an adult is about 8 cubic centimeters.
The ethmoid sinuses look like cells corresponding to the level of the middle and superior turbinates. They make up the upper part of the lateral wall of the nasal cavity. The cells communicate with each other.
 The main sinus is localized in the body of the main bone. In the midline, the cavity is divided by a septum into right and left parts. The sinus opening opens into the upper nasal passage. Some people lack this paranasal sinus.
The main sinus is localized in the body of the main bone. In the midline, the cavity is divided by a septum into right and left parts. The sinus opening opens into the upper nasal passage. Some people lack this paranasal sinus.
The functional significance of these bone cavities lies in the fact that they:
- enhance vocal resonance;
- play the role of a shock absorber when mechanically acting on the cranium;
- isolate the sensitive optic nerves and roots of the teeth from sudden temperature fluctuations caused by inhalation and exhalation;
- moisturize and warm the inhaled air;
- respond to changes in environmental pressure as an additional receptor;
- slightly reduce the weight of the facial bones of the skull, given their large volume.
Indications and contraindications for the appointment of the procedure
The attending physician directs the patient to conduct an ultrasound examination of the paranasal sinuses in the presence of the following symptoms:
- persistent rhinitis of unknown origin;
- periodic nosebleeds of unexplained etiology;
- pain in the sinus areas;
- atypical nasal discharge.
Suspicion of pathology and disease of the paranasal sinuses objectively requires a diagnostic examination. The indications for ultrasound of these bone formations are:
- rhinitis;
- frontitis;
- sinusitis;
- labyrinthites;
- sinusitis;
- adenoiditis.
 All of these diseases can affect the sinus cavities. Given their location and complex structure, as well as the fact that degenerative processes can negatively affect the state of the brain due to the proximity of its localization, if one of the listed diseases is suspected, the attending physician will refer the patient to an echosinusoscopy.
All of these diseases can affect the sinus cavities. Given their location and complex structure, as well as the fact that degenerative processes can negatively affect the state of the brain due to the proximity of its localization, if one of the listed diseases is suspected, the attending physician will refer the patient to an echosinusoscopy.
In addition, this type of diagnosis is often required:
- allergic lesions associated with the appearance of the common cold;
- tumors of any nature, such as polyps or lipomas;
- damage and curvature of the nasal septum;
- the presence of foreign bodies in the sinuses or nasal passages;
- trauma to the corresponding bones of the skull, trauma to the nose.
The patient can be sent for the procedure, or. Indeed, when performing some dental procedures involving the upper jaw, the dental specialist may need the results of echosinusoscopy.
As for contraindications, doctors do not name absolute prohibitions on ultrasound of the paranasal sinuses. The procedure is prescribed with caution to pregnant women. Despite the fact that there is no objective evidence of potential harm to the fetus from scientists, it is believed that, if possible, pregnant women should avoid examinations associated with any kind of radiation, at least during the first trimester of pregnancy. However, ultrasound examinations are almost the only non-invasive diagnostic method that is prescribed to most pregnant women with minimal exceptions.
Children's age is not a contraindication to the appointment of the procedure - ultrasound of the paranasal sinuses is allowed to be performed even for newborns.
The preparation process and technique for performing echosinusoscopy
A diagnostic session using the properties of ultrasonic waves does not require special training from the patient. Food and liquids can be taken before the examination. If an ultrasound scan is done to a small child, the parents first tell him about the procedure, and tune in to the fact that the diagnosis is painless and there is no need to be afraid of it.
Before the start of the ultrasound, the examinee removes all metal jewelry, takes out piercings and dentures, if any. During the procedure, the patient sits motionless on the couch. In some cases, the diagnostician asks him to lie on his back or stomach. The doctor applies a special gel to the area to be examined.
 The doctor determines the location of the cavity of interest, and sets the sensor according to anatomical landmarks in the area of its projection. In this case, the position of the sensor should be strictly perpendicular to the bone in order to minimize the interference caused by the bone tissue.
The doctor determines the location of the cavity of interest, and sets the sensor according to anatomical landmarks in the area of its projection. In this case, the position of the sensor should be strictly perpendicular to the bone in order to minimize the interference caused by the bone tissue.
The peculiarity of the method is that the cavities are visualized on the monitor only if there is content in them, otherwise the echogenic signal is reflected from the air-bone border.
For this reason, in the process of performing an ultrasound scan, the doctor asks the examinee to change the position of the head, for example, bend it forward or throw it back in order to change the border of the location of the liquid, if any.
Ultrasound examination of the paranasal sinuses takes no more than 10-15 minutes and is absolutely painless.
Interpretation of the results of diagnostics of the paranasal sinuses
As a result of visualization of the image of the examined cavities, the doctor has the opportunity to examine them from different angles and analyze their condition. The diagnostician assesses the thickness of the vascular septa, the characteristics of the cartilaginous tissue, the condition of the subcutaneous tissue, the quality of blood circulation. In addition, the doctor determines the presence or absence of neoplasms.
The normal state of the sinuses is not displayed in any way on the monitor of the ultrasound machine, therefore such a study is uninformative, while pathologies and diseases are quite clearly visualized in the image. For example, sinusitis can be detected by changes in mucosal thickness and density caused by edema. A fluid with homogeneous or heterogeneous echogenicity is visible inside the sinus. Cysts and polyps in cavities appear as structures with low echogenicity.
Together with ultrasound, the attending physician often prescribes Doppler ultrasound. By the combination of these procedures, it is easier for a physician to establish an accurate diagnosis.
After examining the results of the ultrasound examination, the diagnostician draws up a conclusion, which, together with the ultrasound images, is issued to the patient. These medical documents must be handed over to the attending physician in order for him to develop tactics of treatment measures, or to assess the degree of effectiveness of the treatment already carried out.
Advantages and disadvantages of the ultrasound method
Of course, the diagnostic ultrasound method has a number of positive characteristics, due to which it is prescribed almost more often than all other types of examinations.
The procedure usually takes 10-15 minutes, while other methods of examination may take longer than an ultrasound scan. In cases where the doctor urgently needs to obtain information about the condition of the patient's paranasal sinuses, any delay is impractical and can be dangerous.
Other scanning techniques do not allow determining the presence and localization of foreign bodies in cavities - this is possible only with the help of ultrasound. Considering that such a problem is often encountered in young children who like to learn about the world in such a traumatic way, the value of an ultrasound examination for them cannot be overestimated.
Scanning with an ultrasound probe is absolutely painless, and does not cause discomfort for the patient, no special preparation is required before starting it.
The safety of ultrasound examination ensures that the procedure can be performed regularly every time it becomes necessary. X-ray or computed tomography cannot boast of such a property.
However, the method also has known disadvantages. Echo-sinusoscopy is an inaccessible type of ultrasound, and not every ultrasound diagnostician has a sufficient level of qualification to carry it out. Some doctors with decades of experience have never faced the need for echosinusoscopy.
In the process of interpreting and decoding the results, the doctor must remember that ultrasound scanning can produce an image with a certain level of error, and in some cases even such a phenomenon as overdiagnosis can occur, that is, a situation when the sensor detects areas with special echogenicity, although no there is no pathology in this place. Often, ultrasound results need to be supplemented with information obtained as a result of other examinations, which requires additional time and costs.
Ultrasound examination of the paranasal sinuses, as a diagnostic method, is highly valued by physicians. Among its advantages are the speed of implementation, sufficient accessibility, in addition, patients note the complete painlessness of the method. Based on the results of the ultrasound scan, the doctor can detect only pathologies or destructive processes in the images - in a normal state, the sinus cavity is not visualized. However, in the presence of polyps or tumors, sinusitis, frontal sinusitis, rhinitis, sinusitis, labyrinthitis, foreign bodies, hemorrhages, the diagnostician will notice characteristic changes in the pictures, and then, if necessary, prescribe additional examinations, establish or confirm the diagnosis, and suggest treatment regimens.
Ultrasound of the maxillary sinuses- a highly specialized examination used in the treatment of ENT diseases. Ultrasound diagnostics of the nose is an affordable and safe alternative to radiography and computed tomography of the maxillary sinuses, however, ultrasound is not always as informative as the above examinations.
With the help of ultrasound of the sinuses, it is possible to determine the presence of fluid or pus in the nasal cavities, the state of all structures (including vascular septa, cartilaginous tissue), the presence of neoplasms of a different nature, foreign objects.
The procedure is completely painless, non-invasive and safe. It can be performed on patients of any age without restrictions, including children and pregnant women. You can do an ultrasound of the nose for a child at any age.
Indications
Ultrasound examination of the maxillary sinuses is effective for diagnosing pathologies of the nasal septum, identifying foci of inflammation in sinusitis, frontal sinusitis, rhinitis, sinusitis. Ultrasound of the nasal cavity is used to study the causes of nosebleeds, allergic reactions, in the presence of polyps, lipomas, the consequences of mechanical damage, as well as in dental practice.
Preparation
The session itself lasts 10-15 minutes, no preliminary preparation is needed. If necessary, ultrasound of the maxillary sinuses is prescribed again to monitor the dynamics of treatment or combined with other diagnostic examinations.
More details
Price
The cost of ultrasound of the maxillary sinuses in Moscow ranges from 600 to 6200 rubles. The average price is 1,410 rubles.
Where to do an ultrasound of the maxillary sinuses?
Our portal contains all the clinics where you can do an ultrasound of the maxillary sinuses in Moscow. Choose a clinic that is suitable for the price and location, and make an appointment on our website or by phone.

What is the Android status bar?
How to choose a gift for the new year for yourself
How to choose gifts for the New Year?
Excel status bar options What the status bar is for
Complete Lessons - Knowledge Hypermarket